Planter heel pain: planter fascitis, Fat pad atrophy, combined PF & FPA.
What the following article is on?Discussion on 3 conditions with mostly similar symptom of planter heel pain.
Synonyms of planter heel pain: Subcalcaneal heal pain, calcaneodynia etc.
Synonyms of Planter fascitis: Planter fasciosis, Planter fasciopathy etc.
Planter foot pain is seemingly the most innocuous yet significant morbid condition affecting the adults hampering their ADLs & QOL. According to a recent research paper (1) Plantar heel pain can be provoked by PF (Planter fascitis), FPA (Fat pad atrophy), combination of PF + FPA and other causes. Patients with PF or FPA typically show different characteristics in clinical features but overall may look quite similar. Plantar heel pain requires differential diagnosis for appropriate treatment.
DD of planter foot pain includes following:
Planter heel pain can be sub-divided in to neural & non-neural pain. The non-neural pain can again be sub-divided into 2 bony & soft tissue pains.
Bony pathology: Calcaneal stress fracture, apophysitis of the calcaneus (Sever's disease), osteomyelitis, or inflammatory arthropathy.
Soft tissue pathology: Fat pad atrophy (FPA) or contusion, plantar fascia rupture and plantar fasciitis (PF).
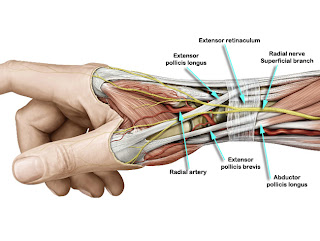
Neural pathology: Entrapment or compression of the first branch of the lateral plantar nerve (Baxter's nerve), medial calcaneal branch of posterior tibial nerve, or nerve to abductor digiti quinti muscle.
Other neural causes include S1 radiculopathy, tarsal tunnel syndrome, and peripheral neuropathy.
Many times planter foot pain is due to combination of different pathologies coexisting together. For example it is reported that Planter fascitis & fat pad atrophy coexist to produce planter foot pain. Similarly Labib et al described the heel pain triad (HPT). HPT is a combination of plantar fasciitis, posterior tibial tendon dysfunction and tarsal tunnel syndrome.
We are going to discuss S/S of 2 different pathologies with similar presentation and they often coexists.
A. Planter fascitis (PF):According to Buchbinder (5) PF is reported to be the most common cause of plantar heel pain. The peak age is between (40-60) years.
Pathology of PF(6):
The pathology is still unknown.
Histopathologic examination of biopsy specimens from patients undergoing excessive extension or microinjuries of the plantar fascia shows secondary degenerative changes in the plantar fascia, with or without fibroblastic proliferation, and without acute inflammation.
However there is aging caused physiological changes are thought leading to PF. There is increased stress on the calcaneus and plantar fascia due to of loss of buffering tissue such as water and collagen of the fat pad.
Risk factors for PF:
1. running excessively (or suddenly increasing running distance)
2. occupations that involve long periods of standing
3. pes planus
4. limited ankle dorsiflexion
5. obesity
Basis of clinical diagnosis:1. Pain characteristics: first-step morning pain and relief of pain after walking (most significant finding). Medial calcaneal tuberosity pain must be view is association with morning 1st step pain to diagnose PF. Unilateral pain is more common than bilateral.
2. Association with abnormal foot biomechanics: TA tightness & Limited ankle DF is most commonly associated with PF. Both pes planus & Cavus are associated with PF however Pes palnus is more associated with PF than pes cavus.
Explanation of association of pes planus & TA tightness with PF:
Limited ankle dorsiflexion on the involved side significantly increased the risk of PF. According to Inman et al (7) approximately 10 degrees of ankle dorsiflexion with the knee extended is required during a normal gait. If the Achilles tendon is shortened, limiting ankle dorsiflexion, excessive pronation of the foot may occur to compensate for this limitation. Greater the limitation in ankle dorsiflexion, the more load on the plantar fascia. Excessive pronation of the foot increases tensile loads on the plantar aponeurosis.
Hence repetitive pronatory stress that increases tensile force on the plantar fascia causing the plantar arch to lower is the cause of PF. The pronatory effect increases with age, and is related to limited ankle dorsiflexion caused by decreased elasticity of the tendons, and the reduced range of motion that occurs with age.
Digiovanni et al (8) reported relief or absence of plantar heel pain in 52% of patients participating in exercises to stretch the plantar fascia, and 22% after stretching the Achilles tendon. This provides a good target for treatment.
3. Heel spur: Heel spur is a common incidental finding in PF than FPA.
Diagnosis on the basis of US scanning:
Hypoechoic fusiform-shaped swelling more than 4 mm in thickness at the origin of the plantar fascia.
B. Fat pad atrophy (FPA):There is loss of buffering tissue such as water and collagen of the fat pad under the heel mostly due to age. The fat pad atrophies and shock absorbency diminishes in subjects that were older than 40 years. Yi et al (1) used the following criteria to diagnose FPA. FPA is said to the causing planter heel pain if more than 3 of the following criteria are present:
1. pain at heel center or margin
2. worsening pain when barefoot
3. worsening pain after a long period of standing
4. palpable calcaneus
In addition to the above following US scan finding: when the patient had a fat pad that was less than 3 mm in thickness.
S/S:
1. B/L pain is common than U/L.
2. Pain characteristics:
a. aching pain (commonest) but also tingling, cold (5.4%) and burning sensations. (highest to lowest in that order)
b. pain after a long walk, pain at night and resting pain (highest to lowest in that order).
3. Both pes planus & cavus are associated with FPA.
4. Risk factors of FPA: B/L pain which get more severe with prolonged standing is likely to be caused by FPA.
C. PF+FPA (PFFPA): PF and FPA may share very similar symptoms and are difficult to distinguish from one another further it has been seen. PF can be co-morbid with FPA. PFFPA shares features common to both PF & FPA. In case of mixed characteristics of PF and FPA, PFFPA should be considered first and ultrasonography should be used as an key diagnostic tool.
Treatment options:
It is imperative to diagnose correctly among seemingly similar S/S in planter foot pain. Many FPA & PFFPA cases are misdiagnosed as having PF and treated with conservative therapy including local steroid injection. In cases treated with steroid to PF there are reports of planter fascia rapture in running, hence it is cautioned to diagnose correctly & treat aptly.
Though many surgical options are available including minimal invasive techniques, there are myriad non-surgical techniques available. Nevertheless, nonsurgical management of plantar fascitis (a predominate cause of planter heel pain) is successful in approximately 90% of patients (2). The options in physical medicinesfor planter heel pain includes: rest, massage, nonsteroidal anti-inflammatory drugs, night splints, heel cups/pads, custom and off-the-shelf orthoses, injections, casts, and physical therapy measures such as shock wave therapy (2). Stretching exercises of the plantar fascia and Achilles tendon can also relieved pain (1). In many studies standing TA stretching is compared with stretching through a prefabricated night splint. Findings suggest that stretching through a prefabricated night splint is a very good option in managing planter foot pain from PF that also is claimed to speeding up the time to recover (4). Heel cushions, heel cups, or low-dye taping can be applied to relieve the pressure on the calcaneus of FPA patients. In those involved in sports correction of training errors and orthotics are essential components in any treatment program (3).
Surgical treatment should be considered in only a small subset of patients with persistent, severe symptoms refractory to nonsurgical intervention for at least 6 to 12 months (2).
References:
1. Yi TI et al; Ann Rehabil Med. 2011 Aug;35(4):507-13. Epub 2011 Aug 31. Clinical characteristics of the causes of plantar heel pain.
2. Neufeld SK et al; J Am Acad Orthop Surg. 2008 Jun;16(6):338-46. Plantar fasciitis: evaluation and treatment.
3. Ryan J; Am Fam Physician. 1995 Sep 1;52(3):891-8, 901-2. Use of posterior night splints in the treatment of plantar fasciitis.
4. Barry LD et al; J Foot Ankle Surg. 2002 Jul-Aug;41(4):221-7. (A retrospective study of standing gastrocnemius-soleus stretching versus night splinting in the treatment of plantar fasciitis.
5. Buchbinder R. Clinical practice. Plantar fasciitis. N Engl J Med. 2004;350:2159–2166.
6. Lemont H, Ammirati KM, Usen N. Plantar fasciitis: a degenerative process (fasciosis) without inflammation. J Am Podiatr Med Assoc. 2003;93:234–237.
7. Inman VT, Ralston HJ, Todd F. Human walking. 2nd ed. Baltimore: Williams & Wilkins; 1994. pp. 45–72.
8. Digiovanni BF, Nawoczenski DA, Malay DP, Graci PA, Williams TT, Wilding GE, Baumhauer JF. Plantar fascia-specific stretching exercise improves outcomes in patients with chronic plantar fasciitis. A prospective clinical trial with two-year follow-up. J Bone Joint Surg. 2006;88:1775–1781. [PubMed]

Comments
Post a Comment