The SI joint pain- Truth of provocative tests & SI joint blocks
Because pain caused by sacroiliac joint dysfunction can mimic discogenic or radicular low back pain diagnosis of sacroiliac joint dysfunction is frequently overlooked, as common practice is to the link low back pain with protruding disc even when neurological signs are absent (1).
The prevalence reported of SI joint caused pain is some where between
1. International Association for the Study of Pain (IASP) criteria demonstrated the prevalence of pain of sacroiliac joint origin in 19% to 30% of the patients suspected to have sacroiliac joint pain.
2. Hansen et al: the sacroiliac joint has been shown to be a source of pain in 10% to 27% of suspected cases with chronic low back pain utilizing controlled comparative local anesthetic blocks.
3. Rupert et al: prevalence of sacroiliac joint pain is estimated to range between 10% and 38%
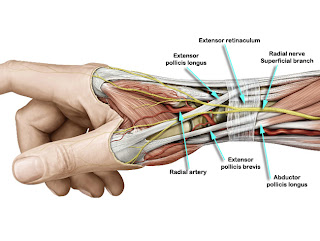
SI joint anatomy:
The sacroiliac joint is a diarthrodial (freely moveable joint) synovial joint with abundant innervation and capability of being a source of low back pain and referred pain in the lower extremity (6).
1. The SI articulation: The joint differs with others in that it has fibrocartilage in addition to hyaline cartilage, there is discontinuity of the posterior capsule, and articular surfaces have many ridges and depressions (2).
2. The SI innervation: The sacroiliac joint is well innervated. Histological analysis of the sacroiliac joint has verified the presence of nerve fibers within the joint capsule and adjoining ligaments. It has been variously described that the sacroiliac joint receives its innervation from the ventral rami of L4 and L5, the superior gluteal nerve, and the dorsal rami of L5, S1, and S2, or that it is almost exclusively derived from the sacral dorsal rami (2).
Diagnosis of pain from SI origin
Mapping studies of pain elicited by injections into the sacroiliac joints (SIJs) suggest that sacroiliac joint syndrome (SIJS) may manifest as low back pain, sciatica, or trochanteric pain (3).However, earlier authors are skeptic about pain from SI joint. Difference in opinion exists between manual medicine practitioners & main stream physicians. Manual medicine practitioners have described many dysfunctions in SI region & pain arising from it. They advocate “cluster testing” for SI joint dysfunctions. Cluster testing refers to a group of physical tests that filters out the SI joint pain from others & it also indicates the type of SI dysfunction.
However it is true that not much exploration is done about the joint. There are no definite historical, physical, or radiological features to provide definite diagnosis of sacroiliac joint pain. While many authors advocate provocational maneuvers; others suggest accurate diagnosis be made by controlled sacroiliac joint diagnostic blocks.
Neither patient-reported symptoms nor provocative SIJ maneuvers are sensitive or specific for SIJS when SIJ block is used as the diagnostic gold standard. This has led to increasing diagnostic use of SIJ block, a procedure in which an anesthetic is injected into the joint under arthrographic guidance (3).
Questioning the SI block as the diagnostic gold standard
A review by Rupert et al (5) recently in 2009 indicates that the false-positive rate of single, uncontrolled, sacroiliac joint injections is 20% to 54%. This review reveals similar evidence levels as Hansen et al’s (6) review in 2007 i.e.
1. The evidence for the specificity and validity of diagnostic sacroiliac joint injections is moderate (Level -II).
2. The evidence for accuracy of provocative maneuvers in diagnosis of sacroiliac joint pain is limited (Level-III).
The answer why SIJ block has limited value as a diagnostic criteria comes from Berthelot et al’s (3) study. Berthelot et al reported that effects of two consecutive blocks are identical in only 60% of cases, and the anesthetic diffuses out of the joint in 61% of cases, often coming into contact with the sheaths of the adjacent nerve trunks or roots, including the lumbosacral trunk (which may contribute to pain in the groin or thigh) and the L5 and S1 nerve roots (3). These partly explain the limited specificity of SIJ block for the diagnosis of SIJS and the discordance between the pain elicited by the arthrography injection and the response to the block.
This report by Berthelot et al also reveals that the failure of the prevocational tests or anesthetic block is partly due to that fact that extra-articular ligaments contribute to the genesis of pain believed to originate within the SIJs. For example, studies by Vleeming et al (7), Mc Grath et al (8) reveal long posterior sacroiliac ligament is responsible for pain in patients with non-specific low back pain. However Berthelot et al have reported the SIJ ligament which either lock or in allow motion of the SIJ are responsible for pain originating from SIJ. These ligaments are
1. The expansion of the iliolumbar ligaments
2. The dorsal and ventral sacroiliac ligaments
3. The sacrospinous ligaments and
4. The sacrotuberous ligaments
Predictive value of provocative sacroiliac joint stress maneuvers in the diagnosis of sacroiliac joint syndromes:
To prove SIJ block is better diagnostic criteria than SIJ physical provocative maneuver, Slipman et al (4) considered 3 tests. Out of these 3 the most conspicuous are
1. Patrick’s FABER test
2. Tenderness in sacral sulcus
The test battery used by Slipman et al to confirm a positive provocative SIJ test found out 50 patients in their study. When they are tested by SIJ block (patients who had more than 80% pain reduction in VAS by the block was considered a positive SIJ block) they found only 30 out of these 50 patients had positive response to SIJ block. So according to Slipman et al predictive value of SIJ provocative test is around 60%. Hence provocative SIJ maneuvers do not confirm a diagnosis of SIJS. Rather, these physical examination techniques can, at best, enter SIJS into the differential diagnosis.
U.S. Preventive Services Task Force (USPSTF) criteria for SIJ
1. For diagnostic interventions
The outcome criteria include at least 50% pain relief coupled with a patient's ability to perform previously painful maneuvers with sustained relief using placebo-controlled or comparative local anesthetic blocks.
2. For therapeutic purposes
*Outcomes include significant pain relief and improvement in function and other parameters.
**Short-term relief for therapeutic interventions was defined as 6 months or less, whereas long-term effectiveness was defined as greater than 6 months.
Management
Conservative management includes
1. Manual medicine techniques
2. Pelvic stabilization exercises to allow dynamic postural control
3. Muscle balancing of the trunk and lower extremities
Interventional treatments include
1. Intra-articular joint injections
2. Radiofrequency neurotomy
3. Prolotherapy
4. Cryotherapy
5. Surgical treatment.
Intraarticular injections, and radiofrequency neurotomy have been described as therapeutic measures(6). The evidence for intra-articular injections and radiofrequency neurotomy has been shown to be limited in managing sacroiliac joint pain (2,6). Glucocorticoids may diffuse better than anesthetics within these ligaments hence instead of anesthetic blocks, hence Glucocorticoids should be better therapeutic agent. Furthermore, joint fusion (arthrodesis) may result in ligament unloading to reduce pain(3).
References:
1. Weksler N et al; Arch Orthop Trauma Surg. 2007 Dec;127(10):885-8. Epub 2007 Sep 8.
2. Forst SL et al; Pain Physician. 2006 Jan;9(1):61-7.
3. Berthelot JM et al; Joint Bone Spine. 2006 Jan;73(1):17-23.
4. Slipman CW et al; Arch Phys Med Rehabil. 1998 Mar;79(3):288-92.
5. Rupert MP et al; Pain Physician. 2009 Mar-Apr;12(2):399-418.
6. Hansen HC et al; Pain Physician. 2007 Jan;10(1):165-84.
7. McGrath MC et al; Surg Radiol Anat. 2005 Nov;27(4):327-30. Epub 2005 Nov 9.
8. Vleeming A et al; Spine (Phila Pa 1976). 1996 Mar 1;21(5):556-62.

Comments
Post a Comment