The crossed arm MFR & fascial connections that may explain it’s effect


Crossed arm MFR is one of the most important myofascial release practiced today. Possible causes of the crossed arm stretch or bilateral rhomboids stretch leading to radiating pain in non-segmental pattern can be many. The possible explanations are
1. Each vertebra is connected on it’s sides to different muscles. Equal amount of pull keeps vertebral alignment normal. Normal alignment is required for normal functioning of spine during loaded phases.
2. Muscle and fascia are the active and passive tensors respectively. Both are structurally & functionally integrated. Increase in tension of active tensors can lead to increase tension of passive tensors and vice versa. Thus faulty tension transmission can affect function and later on dysfunction & derangement is produced.
3. One region of the spine is connected to the other end of the spine by nuraxis & through musculo-fascial system. Trespassing of the nuraxial system or contracture of the musculo-fascial system at one region may lead to dysfunction & pain in other region by faulty tension transmission during loading.
However, probably more than any thing else it is normalization of fascial tone that leads to it’s effects. This MFR not only affects the regional myofascia (the extra thoracic fascia) but may affect the TLF (thoraco lumbar fascia) & vertebral aponeurosis.
To understand the non segmental pain reference from crossed arm stretch or bilateral rhomboids stretch which is a common form of myofascial release in osteopathic terms we have to look into specific anatomical relationships. Following anatomical discussion helps to throw some light into it
1. The structure of extra thoracic fascia & it’s connections (discussed at the bottom of this article)
2. The thoracolumbar fascia (TLF), role of TLF in load transfer from spine to leg
3. The vertebral aponeurosis
Fascia is not just a regional issue!
Fasciae have long interested clinicians in a multitude of different clinical and paramedical disciplines. There are many function of fascia. One among them is ectoskeletal role as a soft tissue skeleton for muscle attachments. Hence it is important for creating osteofascial compartments for muscles, encouraging venous return in the lower limb, dissipating stress concentration at entheses and acting as a protective sheet for underlying structures. Emphasis is placed on recognizing the continuity of fascia between regions and appreciating its key role in coordinating muscular activity and acting as a body-wide proprioceptive organ. Such considerations far outweigh the significance of viewing fascia in a regional context alone (3).
We would like to share Vleeming et al’s work to make our statement clear in the earlier said context.
The TLF:
Vleeming et al studied the role of the posterior layer of the thoracolumbar fascia in load transfer between spine, pelvis, legs, and arms (1). Thoracolumbar fascia has both cephalic & coulad relationships. Caudal relations of the posterior layer of the thoracolumbar fascia encompasses functional coupling of muscles such as the gluteus maximus, latissimus dorsi, erector muscle, and biceps femoris to the fascia.
Anatomic structures normally described as hip, pelvic, and leg muscles interact with so-called arm and spinal muscles via the thoracolumbar fascia. This allows for effective load transfer between spine, pelvis, legs, and arms as an integrated system.
Further it is speculated that the gluteus maximus muscle and contralateral latissimus dorsi muscle are functionally coupled, especially during rotation of the trunk. In that case, the combined action of these muscles assists in rotating the trunk, while simultaneously stabilizing the lower lumbar spine and sacroiliac joints.
Vleeming’s study also revealed in 1995 that
1. Traction to a variety of muscles cause displacement of the posterior layer of TLF.
2. Superficial lamina of posterior layer of TLF is tensed by contraction of various muscles, such as the latissimus dorsi, gluteus maximus and erector muscle
3. And deep lamina of posterior layer of TLF is tensed by contraction of the biceps femoris.
4. Caudal to the level of L4 (in some specimens, L2-L3), tension in the posterior layer of TLF was transmitted to the contralateral side.
The Vertebral aponeurosis is also not a regional issue:
Vertebral aponeurosis has an intimate relationship with TLF & fascia of muscles present in deep layer of the spine. Let us study how this aponeurosis can affect the understanding coupling of the mechanical forces transmitted through the spine.
Lucas et al did a study (2008) on this specific fascia i.e. vertebral aponeurosis. The vertebral aponeurosis is found in all human beings. This fascia is a thin fibrous layer consisting of longitudinal and transverse connective tissue fibers blended together deep to the latissimus dorsi muscle. Morphometrically, the mean length of the vertebral aponeurosis is 38 cm and the mean width is 24 cm. The mean thickness was 3 mm. There is no significant difference between left and right sides, gender or age with regard to vertebral aponeurosis length, width, or thickness. During manual tension of the vertebral aponeurosis, the tensile force necessary for failure has a mean of 38.7 N.
Relationships:
1. Medial attachments: It attached medially to the spinous processes of the of the thoracic vertebrae
2. Lateral attachments: It attached laterally to the angles of ribs
3. Inferior attachments: It attached inferiorly to the fascia covering the serratus posterior inferior muscle (superficial lamina of the posterior layer of thoracolumbar fascia)
4. Superior attachments: superiorly it ran deep to the serratus posterior superior and splenius capitis muscles to blend with the deep fascia of the neck.
5. At the level of the serratus posterior inferior muscle, the vertebral aponeurosis fused to form a continuous layer descending toward the sacrotuberous ligament covering the erector spinae muscle.
These data add to our understanding of the biomechanics involved in movements of the back.
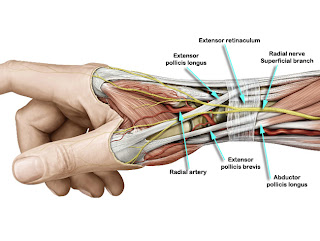
The extra-thoracic fascia & extra-fascial space
The extra-thoracic fascia & it’s spaces holds a significant meaning for dysfunctions affecting this area. The anatomical relationships of this fascia help to understand the impact of the crossed arm MFR.
The pseudo-articulation between the convex posterior rib cage & concave scapula is well described anatomically. There is a plane of cleavage interposed between a posterior muscular plane (levator scapulae, rhomboids, and serratus magnus) and the costo-intercostal surface anteriorly.
This interposed space is bounded by two layers: one is posterior and covers the anterior surface of the rhomboids and the serratus magnus; the second is anterior and rests upon the costo-intercostal surface. This second layer is referred as the "extra-thoracic fascia" by Laterjet et al.
Hence extra thoracic fascia is a continuous fascial layer which covers the surface of the thoracic cage, posteriorly and laterally. The extra-thoracic fascia is independent and can slide smoothly between the muscles and the osteo-muscular wall.
Boundaries & attachments:
Medially -The medial limit originates in the region of the vertebral attachments of the rhomboid and latissimus dorsi, extending to ninth thoracic vertebra.
Laterally -The lateral limit merges at the anterior insertions of the serratus anterior. So lateral limit begin at the lateral portion of the second rib, descends obliquely downwards and anteriorly towards the mid-axillary line, which it reaches at the eighth rib; the lateral limit extends lower than the medial limit.
At lateral and medial limits of the fascia i.e. extra-thoracic fascia merges with the more superficial aponeuroses (see the figure). Thus, in the region of origin of the rhomboid (medial limit of the fascia) there is a continuation with the aponeurosis covering the anterior surfaces of the rhomboid, which continuous with that of the serratus magnus. The figure also demonstrates a space that separates the anterior muscles of the scapula from the thoracic cage.
Superiorly- Above the scapula it merges superiorly and posteriorly with the aponeurosis of the trapezius. Medially to the scapula the fibres run upwards and posteriorly to merge with the aponeurosis enveloping the levator scapulae. Thus, in addition to the closing off of the space medially and laterally by the medial and lateral limits of the extra-thoracic fascia, its fusion with the aponeurosis of the trapezius and the levator scapu!ae limits the space superiorly.
Inferiorly-The inferior border of the extrathoracic fascia runs parallel to the body of the ninth rib or, less frequently, the ninth intercostal space. Thus its course is obliquely downwards and lateral and it is covered by the anterior surface of the latissimus dorsi medially and of the serratus magnus laterally.
The inferior border is more complex, and here the extra-thoracic fascia divides into two sheets.
(1) The deep sheet, which is thinner than the superficial, merges with the thoraco-lumbar region;
(2) The superficial sheet, more resistant, unites with the anterior part of the aponeurosis of the latissimus dorsi medially and that of the serratus magnus laterally. Thus union with these different aponeuroses inferiorly closes the infero-posterior line of the retro-thoracic space.
Fascial spaces:
Due to the presence of the fascia there are existence of two independent fascial spaces one above & one below the fascial space called the extra-fascial space and the sub-fascial space.
Extra-fascial space- This is a closed space. This lies between the muscular plane of the levator scapulae, the rhomboid, the serratus magnus on the one hand, and the extra-thoracic fascia on the other. According to surgeon Laroquette MD this space is seldom free, more often interrupted by connective tissue adhesions which, in order to expose the posterior aspect of the ribs, must be cut by scissors. This space is a potential area for inflammatory fluid collection & the collection may gravitate even up to the level of 9th rib. As reported by surgeons proliferation of dense connective tissue in this space makes it difficult to find the space again.
By making use of the above description of the extrafascial space, it is possible to follow the evolution of tightness & fascial disfigurement leading to poor postural attitudes, open kinetic & closed kinetic chain disorders spreading cephalically & caudally.
Subfascial space- This is not a closed space. Here the fascia is fastened to the muscles with which it is in contact. Above and below it communicates freely with the following regions.
a. Above it opens into the space beneath the superficial cervical aponeurosis, and, by a narrow opening, communicates with the space which separates the first digitation of the serratus magnus from the superior fibres of the serratus posterior superior.
b. Below it continues into the region beneath the muscles of the thoraco-lumbar region, inferior to the ninth rib.
References:
1. Vleeming A et al; Spine (Phila Pa 1976). 1995 Apr 1;20(7):753-8. (The posterior layer of the thoracolumbar fascia. Its function in load transfer from spine to legs.)
2. Loukas M et al; Surg Radiol Anat. 2008 Mar;30(2):125-9. Epub 2007 Dec 18. (Anatomy and biomechanics of the vertebral aponeurosis part of the posterior layer of the thoracolumbar fascia.)
3. Benjamin M; J Anat. 2009 Jan;214(1):1-18. (The fascia of the limbs and back--a review.)
4. Laterjet M et al; Thorax (1953), 8, 282. (An anatomical & surgical sudy of extra thoracic fascia.)
* This article is not exactly corroborative but people who are dealing with this MFR may find important clues how does this MFR work.

Comments
Post a Comment