Understanding Inter-vertebral disc & generation of pain from it
* The interveretbral disc is referred as disc in this following text
Introduction:
The intervertebral discs lie between the vertebral bodies, linking them together. The components of the disc are nucleus pulposus, annulus fibrosus and cartilagenous end-plates. The blood supply to the disc is only to the cartilagenous end-plates. The nerve supply is basically through the sinovertebral nerve. Biochemically, the important constituents of the disc are collagen fibers, elastin fibers and aggrecan. (3)
The role that abnormalities play in the etiopathogenesis of different disorders is not always clear. Disorders may be caused by a genetic predisposition or a tissue response to an insult or altered mechanical environment. According to Roberts et al (2006), whatever the initial cause, a change in the morphology of the tissue is likely to alter the physiologic and mechanical functioning of the tissue (2) which is very important from all varieties (medicinal, physical therapy or surgical) of treatment prospective.
Upcoming new therapies are focusing on to substitute the biochemical constituents, or augment nucleus pulposus or regenerate cartilaginous end-plate or finally artificial disc implantation (3). Let us discuss IV disc & it’s pathologies.
The disc
1. Disc the facilitator of spine movement & flexibility: The intervertebral disc is a highly organized matrix laid down by relatively few cells in a specific manner. The central gelatinous nucleus pulposus is contained within the more collagenous anulus fibrosus laterally and the cartilage end plates inferiorly and superiorly. The anulus consists of concentric rings or lamellae, with fibers in the outer lamellae continuing into the longitudinal ligaments and vertebral bodies. This arrangement allows the discs to facilitate movement and flexibility within what would be an otherwise rigid spine (2).
2. Ageing related developmental considerations of the disc:
a. At birth, the human disc has some vascular supply within both the cartilage end plates and the anulus fibrosus, but these vessels soon recede, leaving the disc with little direct blood supply in the healthy adult (2).
b. With increasing age, water is lost from the matrix, and the proteoglycan content also changes and diminishes. The disc-particularly the nucleus-becomes less gelatinous and more fibrous, and cracks and fissures eventually form. More blood vessels begin to grow into the disc from the outer areas of the anulus. There is an increase in cell proliferation and formation of cell clusters as well as an increase in cell death. The cartilage end plate undergoes thinning, altered cell density, formation of fissures, and sclerosis of the subchondral bone (2).
3. Aging and degeneration are separate processes or the same? In point number 2 mentioned above aeging related developmental changes are considered. The changes described above are similar to those seen in degenerative disc disease. Hence question arises that as to whether aging and degeneration are separate processes or the same process occurring over a different timescale.
4. Separate pathological processes manifests separately: Disorders involving the disc manifests different changes in morphology. They are as follows:
a. Discs in patients with spinal deformities such as scoliosis: These discs have ectopic calcification in the cartilage end plate and sometimes in the disc itself. Additionally discs cells from patients with spondylolisthesis have been found to have very long cell processes.
b. Discs in patients with spondylolisthesis: cells from patients with spondylolisthesis also have been found to have very long cell processes.
c. Cells in herniated discs: Cells in herniated discs appear to have a higher degree of cellular senescence than cells in nonherniated discs and produce a greater abundance of matrix metalloproteinases.
5. Insight into vertebral disc nutrition & basis of disc disintegration- The disc is avascular, and the disc cells depend on diffusion from blood vessels at the disc's margins to supply the nutrients essential for cellular activity and viability and to remove metabolic wastes such as lactic acid. The nutrient supply can fail due to changes in blood supply, sclerosis of the subchondral bone or endplate calcification, all of which can block transport from blood supply to the disc or due to changes in cellular demand (1).
Urban et al (1); reviewed studies on disc blood supply, solute transport, studies of solute transport in animal and human disc in vitro, and of theoretical modeling studies that have examined factors affecting disc nutrition. The results emerged as follows:
a. Role of Diffusive transport & Convective transport: Small nutrients such as oxygen and glucose are supplied to the disc's cells virtually entirely by diffusion; convective transport, arising from load-induced fluid movement in and out of the disc, has virtually no direct influence on transport of these nutrients.
b. Disparity of Diffusive transport & Convective transport leads to: Steep concentration gradients of oxygen, glucose, and lactic acid across the disc; oxygen and glucose concentrations are lowest in the center of the nucleus where lactic acid concentrations are greatest.
The actual levels of concentration depend on the balance between diffusive transport and cellular demand and can fall to critical levels if the endplate calcifies or nutritional demand increases.
c. The result of disparity of Diffusive transport & Convective transport is disc degeneration: Loss of nutrient supply can lead to cell death, loss of matrix production, and increase in matrix degradation and hence to disc degeneration.
6. Disc neurobiology & pain generation:
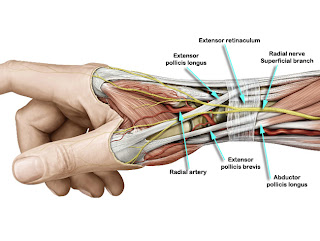
The sinu-vertebral nerve: In the healthy cases only the outer third of the annulus fibrosus of the intervertebral disc is innervated (6). The main innervation of the intervertebral disc is formed by the sinuvertebral nerves. The sinuvertebral nerves are recurrent branches of the ventral rami that re-enter the intervertebral foramina to be distributed within the vertebral canal (4).
Sinuvertebral nerves are mixed polysegmental nerves and nerve plexuses, each being formed by a somatic root from a ventral ramus and an autonomic root from a grey ramus communicans (4).
Neuronal markers for pain-leading fibres were found in the dorsal region of the annulus, and especially in the posterior longitudinal ligament. The expression of neuronal markers in the sarcolemma of the paravertebral muscles is reduced after discotomy (4).
Routes of sympathetically mediated pain in spine: The discs are innervated via sinu-vertebral nerves. However, research in the 1980s suggested that pain sensation is conducted in part via the sympathetic system. This sympathetically mediated entry of pain sensation is by 2 different routes. One route enters the adjacent dorsal root segmentally, whereas the other supply is non-segmental ascending through the paravertebral sympathetic chain with re-entry for example in lumbar spine through the thoracolumbar white rami communicantes (5). The number of nerve bundles gets reduced by resection of sympathetic trunks (4).
Peculiarity of discogenic pain generation in an injured disc: Nerve ingrowths into the diseased intervertebral disc are found in chronic back pain. Freemont et al reported isolated nerve fibres that express substance P deep within diseased intervertebral discs and their association with pain suggests an important role for nerve growth into the intervertebral disc in the pathogenesis of chronic low back pain (6).
Sensory nerve endings in the degenerative lumbar disc penetrate deep into the disrupted nucleus pulposus, insensitive in the normal lumbar spine. Complex as well as free nerve endings would appear to contribute to pain transmission. The nature and mechanism of discogenic pain is still speculative but there is growing evidence to support a 'visceral pain' hypothesis, unique in the muscloskeletal system (5).
Faustmann (4) has summarised the neuroanatomical basis of discogenic pain as follows:
a. The intervertebral disc receives an extensive innervation, especially the annulus fibrosus.
b. Nerve extension into the nucleus pulposus of the degenerated disc.
c. The sinuvertebral nerve plexuses facilitate a polysegmental signal and pain spreading.
d. The innervation of the intervertebral disc is very high connected with the paravertebral muscles.
e. A local denervation of the paravertebral muscles is associated with post-discotomy syndrome.
References:
1. Urban JP et al; Spine (Phila Pa 1976). 2004 Dec 1;29(23):2700-9.
2. Roberts S et al; J Bone Joint Surg Am. 2006 Apr;88 Suppl 2:10-4.
3. Raj PP; Pain Pract. 2008 Mar;8(1):18-44.
4. Faustmann PM; Z Orthop Ihre Grenzgeb. 2004 Nov-Dec;142(6):706-8.
5. Edgar MA; J Bone Joint Surg Br. 2007 Sep;89(9):1135-9.
6. Freemont AJ; Lancet. 1997 Jul 19;350(9072):178-81.
Class on disc pain mechanism-1

Comments
Post a Comment